Prediabetes is a serious but reversible condition where blood sugar levels are higher than normal but not yet high enough for a type 2 diabetes diagnosis. In India, the prevalence is alarmingly high, with the ICMR-INDIAB study estimating 15.3% of adults affected, contributing to over 136 million people at risk. This silent condition often goes unnoticed, as symptoms are subtle or absent, allowing it to progress undetected. Early detection through screening and lifestyle interventions can prevent or delay type 2 diabetes, reducing risks of heart disease, kidney issues, and other complications common in Indians due to genetic predisposition.
This article draws from authoritative sources like the Indian Council of Medical Research (ICMR), American Diabetes Association (ADA), U.S. Preventive Services Task Force (USPSTF), Mayo Clinic (USA), and NHS (UK) guidelines, adapted to the Indian context. Hospitals like Apollo and Fortis offer accessible screening and management via diabetologists, nutritionists, GPs for blood reports, cardiologists, and orthopedists for related risks.


Why Prediabetes Often Goes Undetected in India
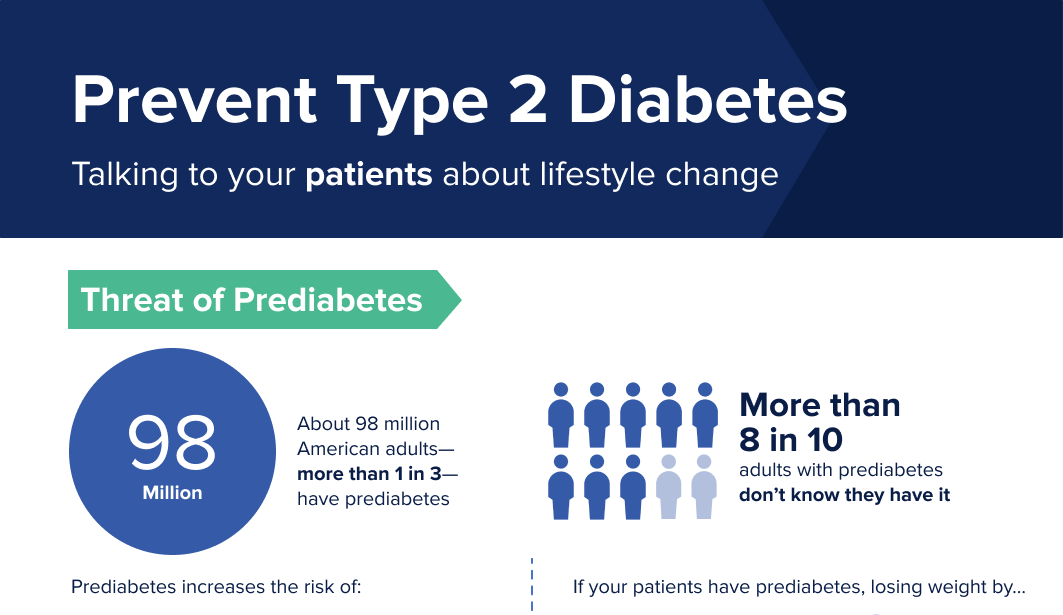
Most people with prediabetes experience no clear symptoms, making it a “silent” threat. ICMR and ADA note that elevated blood sugar (HbA1c 5.7-6.4%, fasting glucose 100-125 mg/dL) can persist for years without notice. In India, high patient volumes and low awareness delay diagnosis, especially in rural areas.
Subtle signs many miss include:
- Persistent fatigue: Feeling unusually tired despite rest, due to cells not getting enough energy from glucose.
- Increased thirst and frequent urination: Excess sugar pulls fluid from tissues, leading to dehydration.
- Blurred vision: High sugar causes lens swelling in eyes.
- Slow-healing wounds or frequent infections: Impaired immune response.
- Dark skin patches (acanthosis nigricans): Velvety darkening on neck/armpits, common in insulin-resistant Indians.
- Tingling or numbness in hands/feet: Early nerve changes.
- Unexplained weight changes or hunger: Despite eating, cells starve for energy.
These are often dismissed as stress, aging, or minor issues. Mayo Clinic emphasizes that without screening, progression to diabetes is likely.

The Impact of Early Treatment on Outcomes
Early intervention dramatically improves outcomes. Studies like the Diabetes Prevention Program (aligned with Mayo Clinic findings) show lifestyle changes reduce diabetes risk by up to 58%, with metformin adding benefits for high-risk individuals.
In India, ICMR guidelines recommend screening from age 30 (earlier with risks like obesity, family history). Reversion to normal glucose is possible:
- Lifestyle changes: 5-7% weight loss, 150 minutes weekly exercise, balanced diet (low refined carbs, high fiber).
- NHS and USPSTF-backed programs show 30-60% reversion rates with brief interventions.
Long-term benefits include lower all-cause mortality, reduced cardiovascular risks, and fewer complications. For Indians, early action counters genetic risks, preventing heart attacks (occurring 5-10 years earlier) and orthopedic issues from diabetes.
Consult a diabetologist for tests (HbA1c, OGTT), nutritionist for diet plans, cardiologist for heart screening, orthopedist if neuropathy affects mobility, and GP for ongoing blood report monitoring.

When to Get Screened and Seek Help
ICMR advises screening >30 years or earlier with risks (obesity, family history, sedentary lifestyle). Apollo and Fortis provide packages including diabetologist consultations and blood tests.
If you notice subtle signs, don’t wait—early treatment changes everything.
Disclaimer: This is general information based on ICMR, ADA, USPSTF, Mayo Clinic, and NHS guidelines. It is not medical advice. Consult qualified professionals like diabetologists or GPs for personalized screening and care.



